A recent study conducted by researchers at Michigan State University has shed light on the reasons behind the prevalence of visceral pain in individuals who have experienced gut inflammation, including those with irritable bowel syndrome (IBS). The study, conducted on mouse models, has shown that glia cells in the nervous system can sensitize nearby neurons, making them more prone to sending pain signals after inflammation occurs. This discovery could pave the way for the development of therapies that can alleviate or eliminate visceral pain by counteracting the sensitizing effects of glia cells.
Currently, there are no medications available in the market that directly target glia cells. However, pharmaceutical companies are actively exploring this approach. Professor Brian Gulbransen, a leading researcher at Michigan State University, is hopeful that this study will provide valuable insights to aid in the development of such treatments.
Notably, the study focused on nociception, which refers to the signals sent by the nervous system in response to physical stimuli. Pain, on the other hand, encompasses the interpretation of these signals in the brain. Gulbransen highlights that while nociception and pain are closely related, they can exist independently of one another. This distinction is important when extrapolating results from animal models to humans.
Despite this caveat, Gulbransen is excited about the significant findings of his team. The study suggests a new mechanism contributing to gut pain, which is one of the most common gastrointestinal issues. The enteric nervous system, also known as the “second brain,” is often overlooked but plays a crucial role in regulating gastrointestinal functions. Similarly, glial cells in the gut have been largely ignored as they are not electrically active, unlike neurons. However, recent advancements in analytical techniques have allowed researchers to study these cells more effectively.
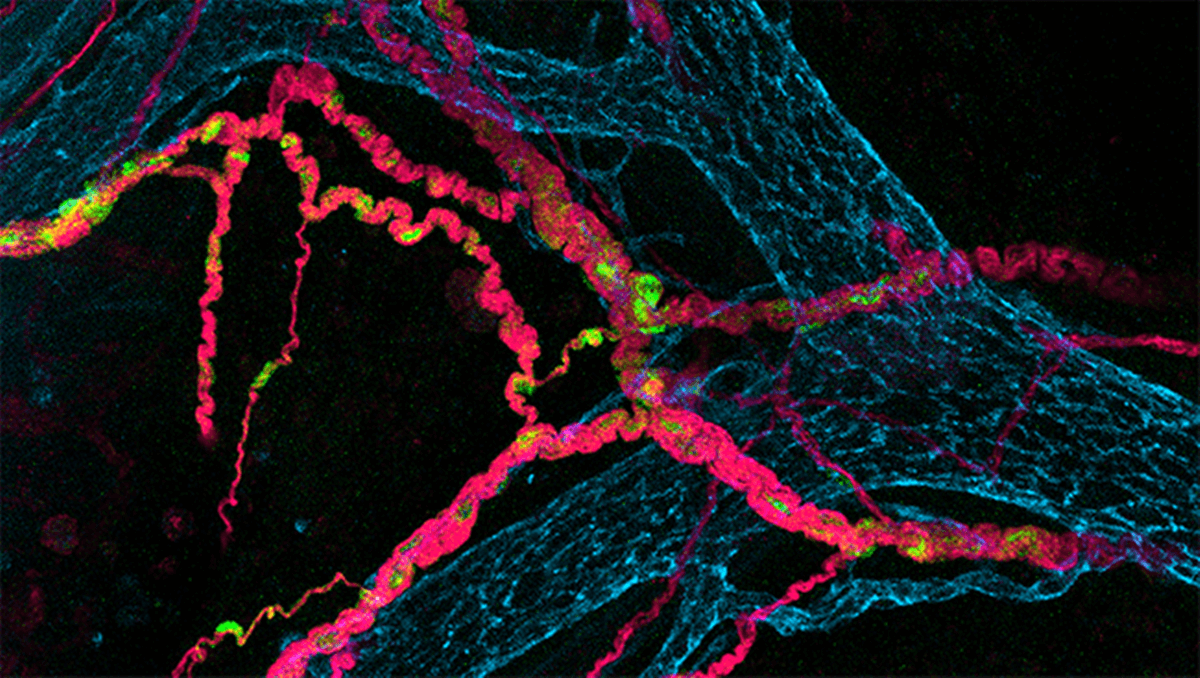
The study revealed that glia cells, when exposed to inflammation, release compounds that alter the chemistry of the gut and sensitize nerve fibers. The research team, led by Wilmarie Morales-Soto, a postdoctoral research fellow at the Mayo Clinic, utilized genetic and chemical techniques to monitor glial cells before and after gut inflammation. The team observed no changes in nerve fiber sensitivity in healthy glia cells. However, inflammation triggered a significant alteration in glia behavior and chemistry, leading to increased nerve sensitivity.
Moving forward, Gulbransen and his team are eager to address more questions surrounding visceral pain. They aim to explore factors such as the higher susceptibility of females to visceral pain compared to males, as well as the impact of early-life adversity, stress, and trauma on pain sensitivity. By understanding the role of glia in these situations, researchers may uncover innovative approaches to treat gut pain and improve the quality of life for individuals suffering from visceral pain.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it