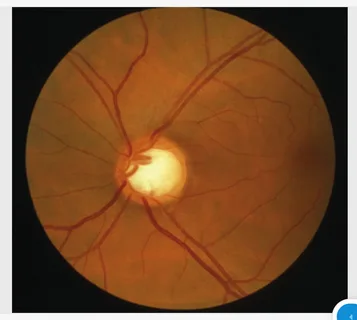
Primary open-angle glaucoma (POAG) stands as the leading cause of blindness among individuals aged 55 and above. Despite its prevalence, a cure for the disease remains elusive, and its underlying biological mechanisms continue to pose a challenge. While elevated intraocular pressure (IOP) is a recognized risk factor for POAG, a significant number of patients afflicted with the condition exhibit normal eye pressure and still experience vision loss.
In a groundbreaking study published in Nature Communications, researchers from Mass Eye and Ear, spearheaded by Ayellet Segrè, Ph.D., embarked on a comprehensive exploration that amalgamated genetic revelations from an extensive cross-ancestry meta-analysis of POAG conducted by Janey Wiggs, MD, Ph.D., along with a sizeable meta-analysis of IOP intertwined with genetic regulation studies and single-cell expression measurements in eye tissues relevant to glaucoma.
Through their meticulous investigation, the researchers unearthed pivotal genes, biological processes, and cell types that could possibly influence the development of POAG either dependent on or independent of IOP levels.
Incorporating integrative analyses, they pinpointed a multitude of genes and regulatory impacts underpinning over 100 loci linked to POAG and/or IOP that could heighten the risk of glaucoma by altering gene expression levels. These genes are enriched in biological pathways associated with disease mechanisms such as elastic fiber formation, extracellular matrix organization, vascular development, and neuronal-related functions.
Moreover, leveraging single-nucleus gene expression data from the aqueous humor outflow pathways, retina, and the optic nerve head alongside the cell atlas of the entire eye guided by Josh Sanes, Ph.D., from Harvard University’s Department of Molecular and Cellular Biology, the scholars identified established and lesser-known cell types where gene dysregulation might impact optic nerve degeneration.
These include fibroblasts in the conventional and unconventional outflow pathways, astrocytes in the retina and optic nerve head, oligodendrocytes and vascular cells in the optic nerve head, and fibroblasts in the adjoining region of the optic nerve head.
The pathways brought to light in their analysis have the potential to influence various eye structures, highlighting various mechanisms that could interact with different genes and cell types contributing to POAG. These revelations offer fresh insights into gene expression and post-transcriptional gene regulation, which could positively influence the design of drugs for treating glaucoma.
Segrè remarked, “Our work has generated new insights into POAG mechanisms, which could inform the development of novel therapies targeting IOP reduction and neuroprotection.” The study suggests that directing attention not only towards retinal ganglion cells but also to neuronal support cells may be crucial in devising innovative drug and cell therapies. The team looks forward to delving further into genetic regulation of gene expression in glaucoma-relevant eye tissues to achieve a more comprehensive understanding of POAG risk and IOP variability.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it