Spinal laminoplasty is a common procedure used to treat spinal stenosis. It aims to prevent or delay further compression of the spinal cord and nerves by expanding the spinal canal. Over the past few decades, it has gained popularity globally as an alternative to laminectomy for treating cervical myelopathy.
History of spinal laminoplasty
The earliest accounts of Global Spinal Laminoplasty date back to the 1940s when Japanese surgeons began experimenting with methods to open the spinal canal from the back rather than removing lamina. In 1976, Kurokawa first published the technique of open-door laminoplasty that is predominantly used today. Since then, various advancements have been made in surgical approaches and implant materials.
By the 1990s, laminoplasty emerged as the preferred alternative to laminectomy in Japan owing to its ability to preserve spinal stability and reduce risks of cervical kyphosis. This prompted its evaluation and adoption in other countries. Today, it is routinely performed worldwide for managing cervical stenosis and ossification of the posterior longitudinal ligament (OPLL).
Surgical techniques
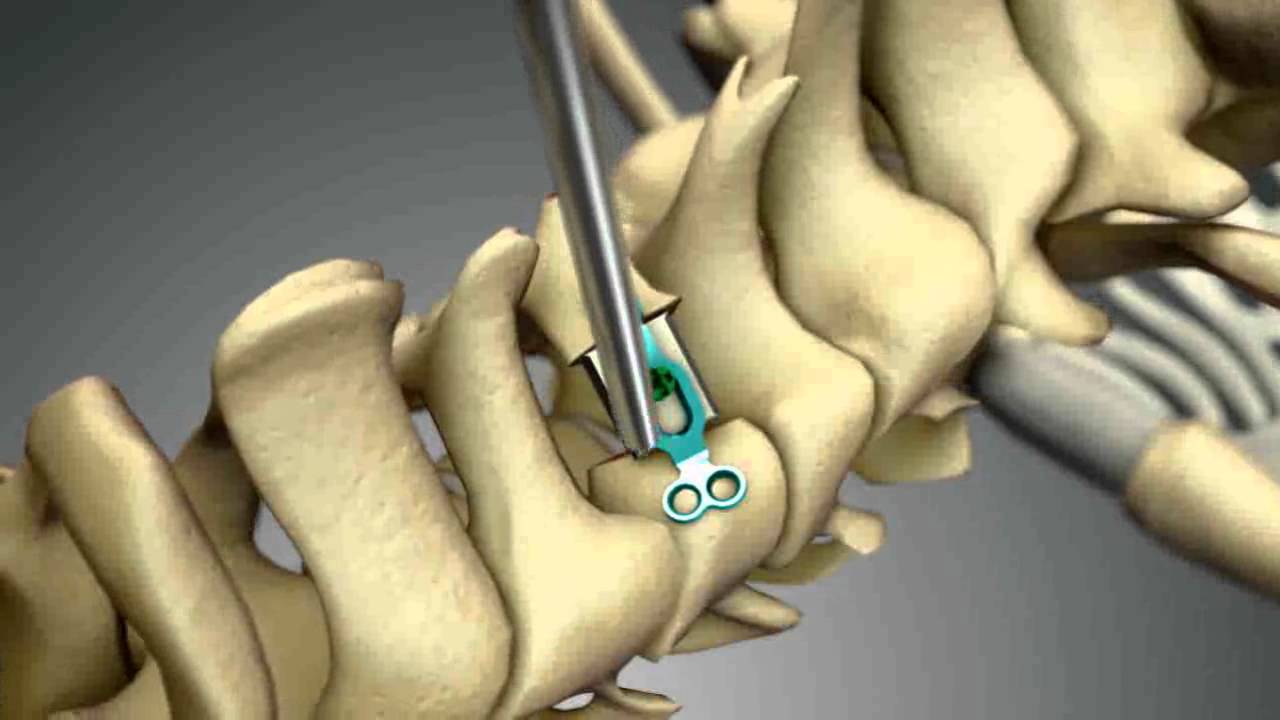
There are several types of laminoplasty techniques based on how the lamina is opened and stabilized. Some common ones include:
– Open-door laminoplasty: It involves creating a hinge on one side of the lamina and rotating it open. The opened lamina is fixed using plates, screws or sutures.
– French-door laminoplasty: Here, a bilateral hinge is made on both sides of lamina which is then opened like a door. Fixation is done using interspinous wiring or miniplates.
– Spinous process-splitting laminoplasty: The spinous processes are split vertically and lamina is opened on both sides. Fixation uses wires passed through the split spinous processes.
– Laminar-saving laminoplasty: This technique aims to preserve the anatomical integrity of lamina by undercutting its inner side to achieve indirect decompression.
Developments in plates and stabilization
Early techniques relied on sutures and wiring for stabilization but had high risks of lamina closure. This led to designing low-profile titanium plates that could lock firmly onto lamina and provide long-term stability.
Notable plate designs include Codman Laminoplasty Plating System (Johnson & Johnson), Solco laminoplasty miniplate system (Stryker) and Mizuho OSI laminoplasty plating system. Bioabsorbable plates are also gaining attention for avoiding implant removal surgery.
Advances in fixation methodology, modular plate designs and low-profile implants have improved stability outcomes and surgical efficacy of laminoplasty globally.
Global statistics
Japan has the highest rates of performing spinal laminoplasty, with over 100,000 annual cases, owing to a greater incidence of cervical OPLL and early adoption of the technique. Other Asian countries like South Korea and China have also extensively adopted it.
European countries saw uptake of laminoplasty from 2000s, though laminectomy remains more common. The US saw a fourfold increase in laminoplasty cases between 1996-2008 according to one study. It is steadily gaining acceptance there for multi-level stenosis.
According to one estimate, over 300,000 laminoplasty procedures are performed annually worldwide for managing cervical myelopathy and ossification. This reflects increasing recognition of its advantages over laminectomy for preserving stability and avoiding late-onset deformity.
However, laminectomy is still preferred in some parts where surgeons lack experience or suitable implants are unavailable. Standardization of techniques and developing econo mic plate designs can boost global laminoplasty rates further.
Decompression outcomes
Clinical studies evaluating laminoplasty report good-to-excellent neurologic recovery rates of 70-90% for arm/hand symptoms and 50-70% for gait disturbances. Several meta-analyses have found laminoplasty to be comparable or better than laminectomy in improving Japanese Orthopaedic Association (JOA) and Neck Disability Index scores.
Imaging studies using MRI also demonstrate satisfactory vertebral canal expansion and indirect dorsal root ganglion decompression following laminoplasty. However, possibilities of late hinge closure or unstable fusion with loss of correction exist in 5-15% cases requiring revision.
New frontiers in research
Future directions for research include developing biomaterials for hinge stabilization, bioabsorbable miniplates and augmented spinal fusion techniques combined with laminoplasty. Nanotechnological coatings on plates may help reduce infection and promote bone fusion.
Robotic and minimally invasive laminoplasty are promising minimally disruptive approaches being evaluated. Stem cell and gene therapies hold potential for enhancing bone fusion after laminoplasty and preventing late closure. Outcomes registries can help standardize techniques and long-term efficacy analysis.
Global adoption of spinal laminoplasty over the past few decades demonstrates its effectiveness as a motion-preserving alternative to laminectomy for various cervical spinal disorders. Continued surgical refinements, development of advanced fixation implants and biomaterials, and evaluation through well-designed studies promise to further establish laminoplasty as the preferred technique worldwide.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it