A groundbreaking study conducted by researchers at the University of Massachusetts Amherst has revealed significant insights into aplastic anemia, a rare autoimmune disorder. This study, published in Frontiers in Immunology, sheds light on the potential for training a specialized subset of cells to counteract the exaggerated immune response responsible for autoimmune disorders. The research has pinpointed an enzyme called PRMT5 as a key regulator of suppressive activity within these cells.
The immune system is a complex mechanism designed to protect the body from pathogens. However, in cases like aplastic anemia, where the immune response is misdirected, severe consequences can occur. Patients with aplastic anemia experience an attack on healthy stem cells in the bone marrow by immune cells known as Th1 cells. This harmful immune response results in the body’s inability to produce crucial blood components like white blood cells, red blood cells, and platelets.
Nidhi Jadon, a graduate student at UMass Amherst and the lead author of the study, explains the goal of creating ultra-suppressive cells to regulate autoimmune disorders without relying on drug interventions. While current drug therapies can be effective, they often come with adverse side effects. By retraining the body’s own defense system, researchers aim to develop a more natural and efficient way to combat autoimmune diseases.
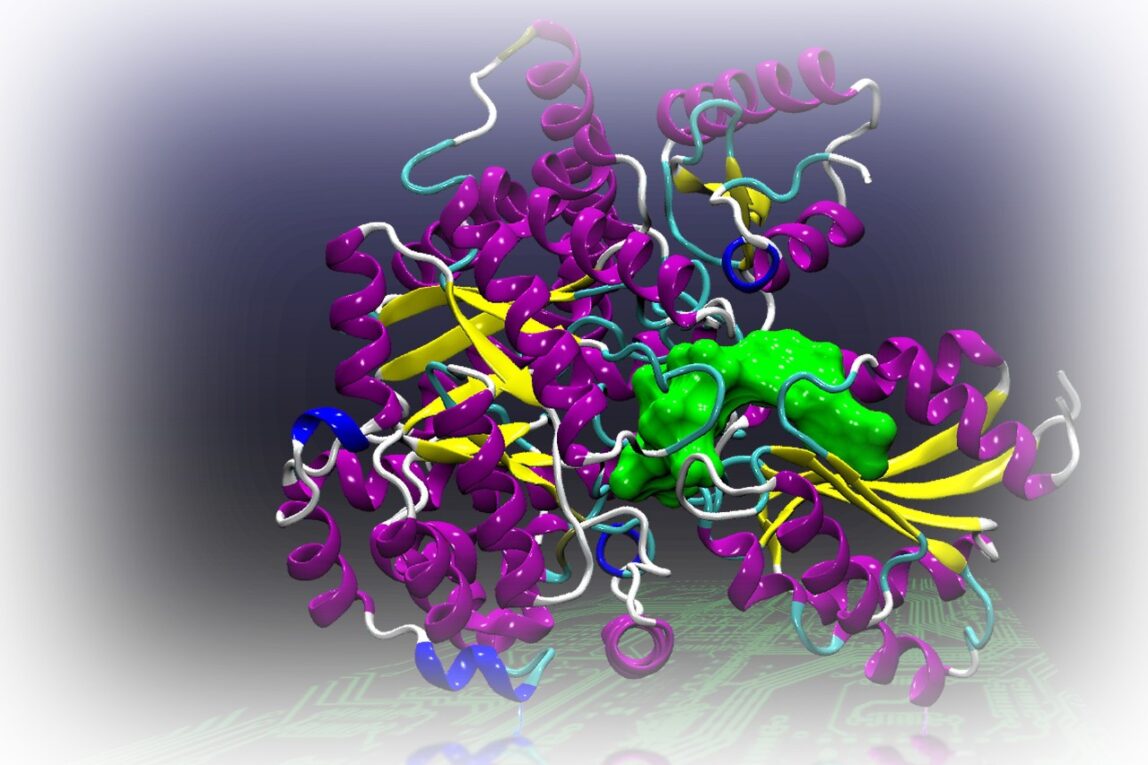
The research team utilized a mouse model developed by Lisa M. Minter in 2013 to mimic the immune responses seen in aplastic anemia. By focusing on training iTregs, cells responsible for suppressing the immune response, in an environment similar to that created by aberrant Th1 cells, the researchers observed promising results. The iTregs demonstrated enhanced effectiveness in reducing the harmful immune response by increasing the production of PRMT5, an enzyme that inhibits the expression of genes destabilizing the suppressive cells.
Minter emphasizes the significance of PRMT5 in enhancing the immune suppressive capabilities of iTregs under conditions resembling a Th1-mediated immune response. Although translating these findings into clinical therapies will require additional research, the team remains optimistic about the potential impact of this discovery. The next steps involve exploring other genes influenced by PRMT5 to further enhance the suppressive abilities of iTregs.
The study’s conclusions from retrained iTregs in mouse models with aplastic anemia showed a notable improvement in survival rates. This progress brings researchers closer to developing super-suppressive cells as a viable alternative to traditional drug treatments. The findings offer new hope for individuals managing autoimmune disorders and pave the way for innovative therapeutic approaches in the future.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it