Causes and Risk Factors of COPD
COPD is mainly caused by long-term exposure to irritating gases or particulate matter, most often from cigarette smoking. About 80-90% of COPD cases are caused by smoking. However, other factors such as secondhand smoke, air pollution, occupational dusts and chemicals may also contribute to the development and progression of COPD. Genetic factors play a smaller role. The risk of COPD increases with the number of years of smoking and number of packs of cigarettes smoked per day. Repeated or severe lung infections during childhood may also increase the risk of COPD later in life. Overall, the greatest risk factor is a history of smoking or exposure to tobacco smoke.
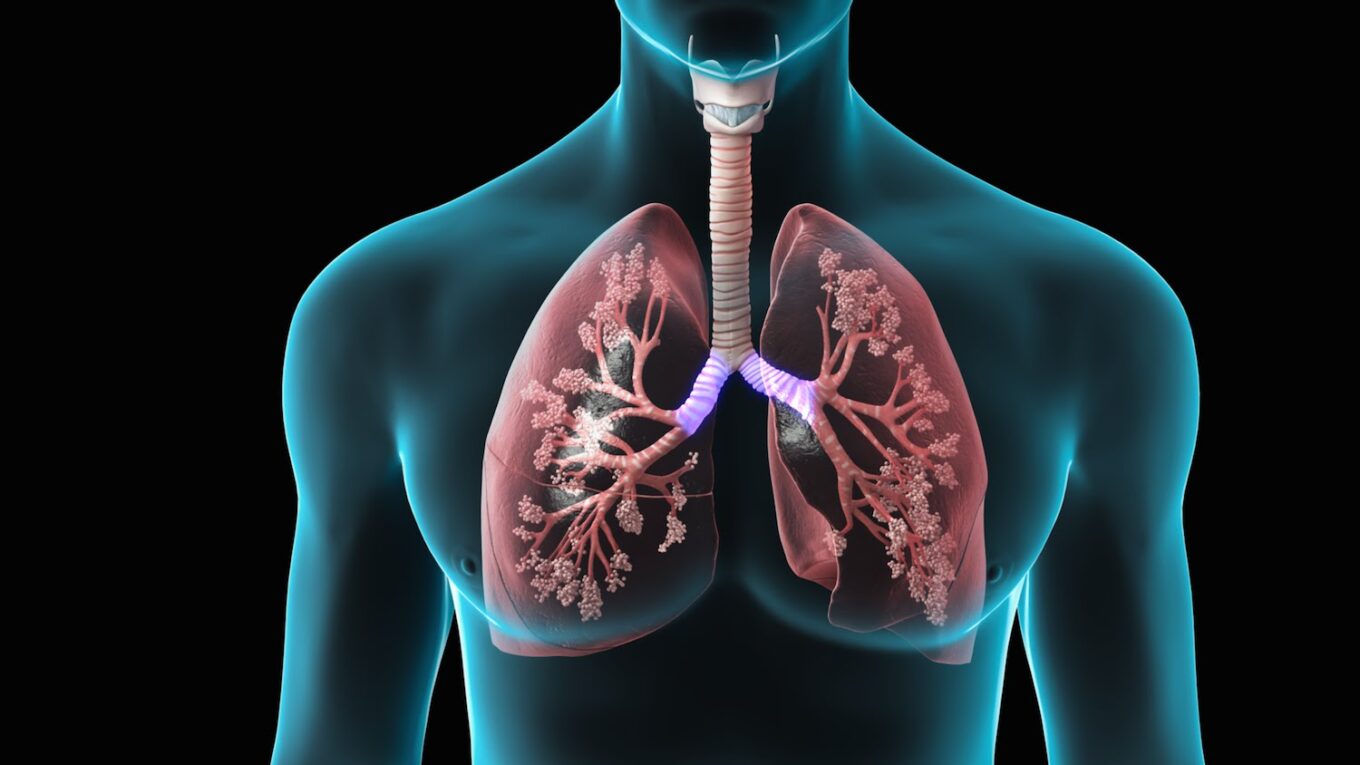
Symptoms of COPD
The main symptoms of Chronic Obstructive Pulmonary Disease (COPD) Treatment include shortness of breath, chronic cough with mucus (sputum) production, and wheezing. These symptoms usually progress slowly over many years. As the disease worsens, the lungs are less able to provide oxygen to the body and remove carbon dioxide. This can eventually lead to severe shortness of breath, even at rest. Other symptoms may include frequent respiratory infections, lack of energy, unintended weight loss, swollen feet or ankles, and depression or anxiety. Severe cases of COPD may result in respiratory failure or heart failure requiring mechanical ventilation or oxygen therapy.
Diagnosis of COPD
COPD is diagnosed mainly based on symptoms and pulmonary function tests. Spirometry, a common breathing test, is used to measure how much air the lungs can hold and exhale by recording the forced expiratory volume in 1 second (FEV1) and the total forced vital capacity (FVC). A reduced FEV1 to FVC ratio below 70% after bronchodilator use confirms the diagnosis of COPD. Chest X-rays may show evidence of hyperinflation and flattened diaphragms in advanced cases but appear normal in mild disease. Further tests like chest CT scans, exercise tests or oxygen saturation studies may be done to evaluate severity and assess treatment needs.
Management of COPD
Current treatment aims to reduce symptoms, improve quality of life and exercise tolerance, prevent worsening of the disease, and minimize risks of complications.
Avoidance of further exposure to irritants like tobacco smoke is crucial. Influenza and pneumonia vaccinations are recommended to prevent infections.
Bronchodilators form the mainstay of therapy. Short-acting bronchodilators like albuterol are used for quick symptom relief as needed. For long-term control, low doses of inhaled corticosteroids may be added for patients with frequent exacerbations. Combination inhalers containing long-acting beta-agonists and corticosteroids together are also commonly used.
Oxygen therapy is required for patients with low oxygen saturation to improve survival and quality of life. Lung volume reduction surgery or valve placement procedures may help some with severe emphysema. Influenza and pneumonia vaccinations are important to prevent infections. Pulmonary rehabilitation programs focusing on exercise, breathing techniques and education help patients manage the disease better. Lung transplants may be considered in very severe cases.
Nutritional support and management of comorbidities such as heart disease are also important aspects of comprehensive COPD care. Medical treatments can’t reverse the lung damage caused by COPD but aim to control symptoms and prevent further worsening of the disease. With proper treatment, most people with COPD can lead an active life.
Non-pharmacological Treatment of COPD
For patients with mild or moderate disease, lifestyle measures and breathing exercises comprise the first-line treatment approach before drugs. Some of these non-drug therapies include:
– Smoking cessation: Completely quitting smoking is the single most important action a person can take to improve their COPD. E-cigarettes,patches or gum with counseling help many patients kick the smoking habit.
– Pulmonary rehabilitation: Comprehensive programs involving exercise training, breathing techniques, nutritional therapy and education empower COPD patients in managing their condition actively at home. Rehab leads to measurable gains in exercise capacity, quality of life, and reduced lung function decline.
– Breathing exercises: Deep breathing and controlled coughing exercises help bring up sputum and increase chest expansion and lung capacity. pursed-lip breathing relaxes the throat and slows rapid breathing.
– Nutrition and diet: Eating a balanced, high-protein and high-calorie diet helps maintain muscle mass and strength in advanced COPD. Oral nutritional supplements provide extra calories and nutrients.
– Avoiding irritants: Staying away from tobacco smoke, dust, smog and chemical fumes protects the lung health further. Use of face masks when exposed helps to some extent.
– Flu shots: Annual flu vaccinations significantly reduce the risks of lung infections, hospitalizations and disease exacerbations in COPD.
– Oxygen therapy: Supplemental oxygen via nasal cannula or masks improves survival and exercise tolerance for those with low oxygen levels. Portable oxygen devices allow mobility.
While non-drug approaches are the first-line management, medicines cannot be avoided as the disease progresses. A combination of lifestyle changes and prescribed inhalers and tablets suits most COPD patients. Compliance with the overall treatment plan enhances clinical outcomes.
Prognosis of COPD
The course and severity of COPD varies greatly among individuals. On average, symptoms worsen gradually over 10-20 years from onset. Disease progression depends on severity of lung damage, exacerbation frequency, adherence to treatment and other health issues. Lung function decline occurs at a rate of around 30-50 ml per year in normal cases. However, smoking, severe underlying emphysema or frequent flare-ups may accelerate loss in lung function.
Long-term oxygen therapy for those qualifying mitigates heart and lung-related complications. Overall, Chronic Obstructive Pulmonary Disease (COPD) Treatment reduces life expectancy by an average of 5 to 10 years. With aggressive treatment, close monitoring, lifestyle control and management of exacerbations, many people can significantly slow disease progression and live good-quality lives. The disease can rarely stabilize or improve in early stages with some patients showing minimal symptoms years on. But smoking cessation must be a priority regardless the level of illness. Timely care including rehabilitation and optimized pharmacotherapy always help maximize quality of life with COPD.
COPD refers to a treatable group of lung disorders characterized by persistent respiratory symptoms and airflow limitation predominantly due to significant airway and/or alveolar abnormalities usually caused by smoking. While symptoms worsen over time once it develops, a combination of lifestyle modifications, medicines, pulmonary rehabilitation and oxygen therapy helps control the disease and its effects. With comprehensive care and management strategies, individuals with COPD can still maintain an active lifestyle and relatively good quality of life.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it