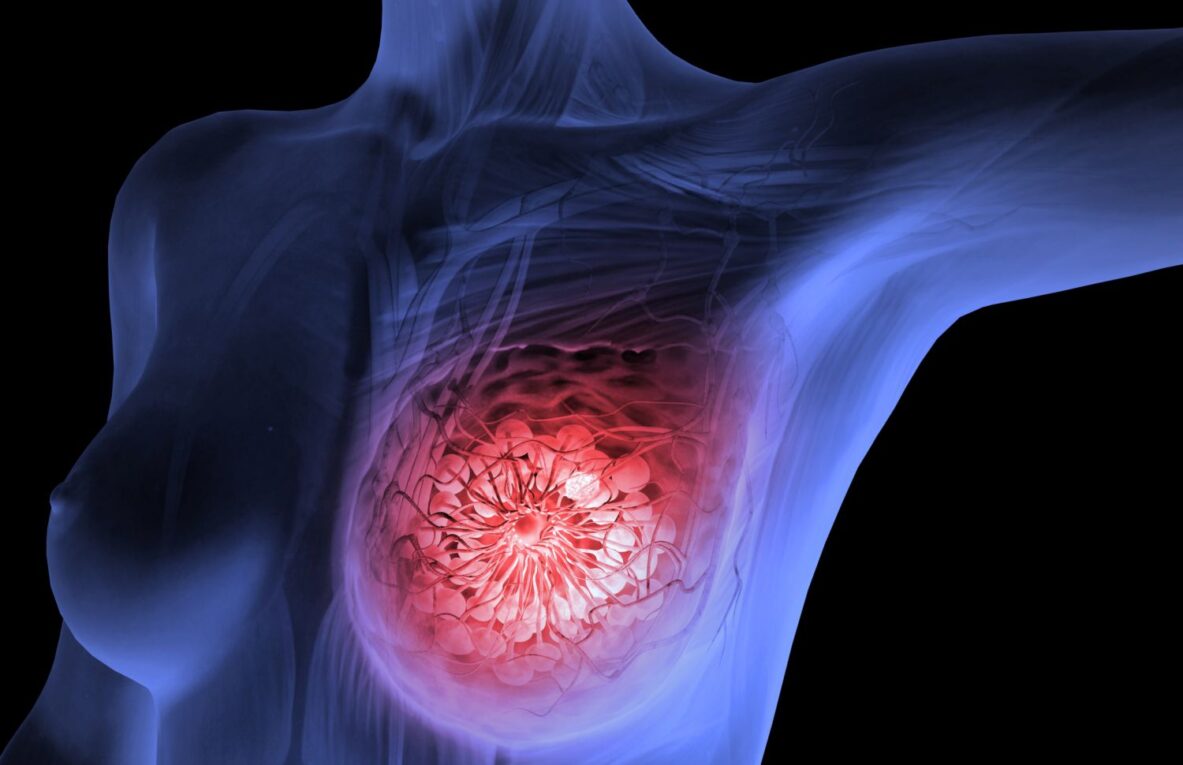
Breast cancer is one of the most common cancers affecting women worldwide. Early detection plays a key role in improving treatment outcomes and survival rates. Breast imaging utilizes different radiological techniques to screen for breast abnormalities at an early stage when treatment is most effective.
Mammography
Mammography is considered the gold standard breast screening tool. It uses low-dose x-rays of the breast tissue to detect small abnormalities that may indicate cancer. Mammograms are often the first test ordered by doctors for women showing symptoms or as part of routine breast cancer screening.
Digital mammography provides high-quality images of the breast tissue on a computer screen. It has replaced traditional film mammography in most centers due to advantages like electronic storage of images and ability to zoom in on suspicious areas. Screen film mammography is still used in some cases.
screening mammograms can detect breast cancers at an early stage, even before physical symptoms appear. Early detection allows for less invasive treatment options and better chances of cure. The American Cancer Society recommends annual screening mammograms for average-risk women starting at age 40. For women at high risk of breast cancer due to family history or genetic mutations, screening may begin earlier.
Breast Ultrasound
Breast ultrasound uses high-frequency sound waves to create images of the breast tissues and structures. It is often used as an adjunct to mammography when something suspicious is seen on mammogram that requires further evaluation. Ultrasound is also useful in women with dense breasts where mammography may not provide clear images.
During an ultrasound exam, a technician spreads ultrasound gel on the breast and moves a handheld transducer over it. The transducer both sends and receives the sound waves to produce images on a monitor. Benign and malignant lesions appear with different characteristics on ultrasound. It can help determine if a suspicious area seen on mammogram is a solid mass or fluid-filled cyst.
Ultrasound is also useful during biopsy procedures to guide the placement of needles into suspicious breast lesions. It poses no radiation risk and is painless, making it a good supplemental or follow-up tool after mammography.
Breast MRI
Breast MRI or magnetic resonance imaging relies on strong magnetic fields and radio waves to generate detailed pictures of breast tissue. It is better than mammography or ultrasound at depicting the internal structures of the breast.
Breast MRI has become an important tool for screening high-risk women who carry gene mutations like BRCA1/2 increasing their likelihood of breast and ovarian cancers. It can also detect cancer in the opposite breast or another area of the same breast in women already diagnosed with the disease. MRI is very sensitive in picking up small lesions but lacks specificity, so additional mammogram or ultrasound may be required.
Breast MRI has a few disadvantages like higher costs compared to other tests, longer scanning time requiring patients to remain still, and possibility of false positive results requiring biopsies. It uses a contrast dye that is safe for most but may cause side effects like nausea in some. However, modern breast MRI with optimized protocols provides highly reproducible exams and an extra level of screening reassurance for women at very high hereditary cancer risk.
Breast CT or Tomosynthesis
3D breast tomosynthesis, also known as breast computed tomography (CT), combines digital mammography with multiple low-dose x-ray images taken of the breast in different angles. These images are reconstructed using computer algorithms into 3D views allowing detection of subtle lesions overlooked on standard mammograms.
The benefits of 3D breast tomosynthesis over 2D mammography include improved accuracy in differentiating malignant lesions from normal overlapping tissues. It provides a 40% increase in cancer detection compared to digital mammograms alone. However, screening using tomosynthesis alone without routine mammograms is still being studied before it can be standardized. At present it is used as an add-on to mammography screening in many centers.
Tomosynthesis poses similar minimal radiation exposure as standard mammography. No extra compression of the breasts is needed compared to additional imaging views taken during diagnostic mammograms. Early patient satisfaction with comfort level during breast tomosynthesis exams has been high.
Positron Emission Mammography
Positron emission mammography (PEM) or PEM-CT is an advanced molecular breast imaging technique providing functional and anatomic data. A small amount of radiotracer (usually fluorodeoxyglucose or FDG) is injected into a patient’s arm vein and concentrated in areas of increased metabolic activity like cancerous tissues.
PEM detects increased uptake of radiotracer in tumors and distinguishes malignant lesions from normal or benign growths more precisely than anatomical imaging alone. The molecular information it provides allows identification of additional areas of cancer spread sometimes missed on usual breast imaging tests.
While PEM shows great promise in improving cancer detection rates over MRI or 3D breast tomosynthesis, it is still not widely available. Studies are ongoing to establish its role in screening high-risk patients, detecting recurrence, or providing tissue characterization data to guide biopsies. As technology advances, cost comes down, and protocols get optimized, PEM can play a bigger supplemental role in breast cancer management in the future.
Choosing the Right Modality
The choice of breast imaging modality depends on individual risk factors, symptoms, lesion characteristics on previous exams, and clinical indication. Mammography remains the standard initial breast cancer screening test. Ultrasound, MRI, tomosynthesis, and newer tools provide added layers of information for specific clinical scenarios. An appropriate combination maximizes cancer detection rates while avoiding unnecessary additional tests or biopsies. An experienced breast radiologist can best recommend the optimal imaging evaluation approach in each case.
Continued research in breast imaging technologies aims to further enhance cancer detection capability while limiting false positives or radiation exposure from repeat scans. Multimodality diagnostic approaches along with artificial intelligence (AI) analysis of images also holds promise to significantly improve radiologists’ assessment abilities. Ultimately, this will benefit early detection efforts and cancer survival statistics worldwide. Annual screening on recommended schedules tailored to risk remains key to breast health.
Breast imaging provides highly effective non-invasive means to screen, detect, characterize and stage breast abnormalities at an early curable stage through different modalities. Regular screening as per guidelines along with prompt clinical and imaging follow-up of any suspicious findings allows timely diagnosis and optimized treatment outcomes. Continued advancements hold continued promise for the future.
*Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it